Top articles of 2021 roundup
What do health plan leaders want to know for 2022?
This year, as with any other year, health plan leaders want to know more about their members: where they are, what they want, and how to connect with them in more meaningful ways. As we dive into 2022 (and the strategic planning that goes with it), we’re highlighting the resources our health plan leaders read most in 2021.
1.
2021 HEALTH PLAN MEMBER IMPACT REPORT:
What’s top of mind for your members?
The more you know about your members, the bigger impact you can have on their health. This quarterly member impact report highlights key member engagement metrics—like touch points per member per month, maternal health insights, and behavioral health support needs. Don’t go into 2022 without understanding what is top of mind for your members and their families.
Read the Member impact report
2.
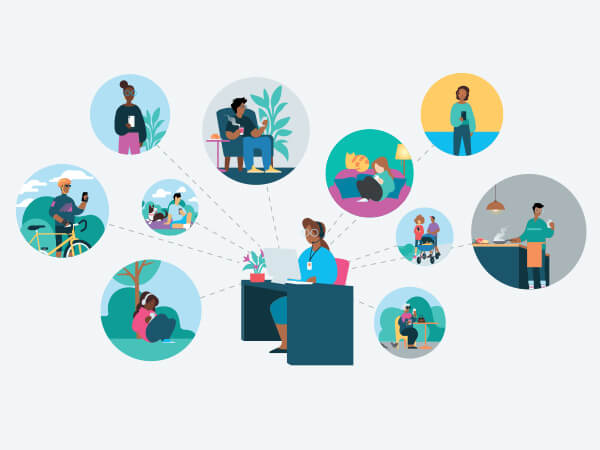
9 digital care management capabilities that scale member engagement
Your health plan needs to reach more members. But how can you do that with the resources you have—and without overloading your staff? This interactive page highlights 9 digital care management tools that can help your plan engage more members in less time. See what digital health capabilities other health plans are using to improve their member experience as well as care outcomes.
Read about the 9 digital care management capabilities

3.
The evolution of telehealth: Digitizing the member journey
Telehealth seemed to be the solution to closing gaps in care after the COVID-19 pandemic began. But telemedicine is still episodic, much like in-person care. To truly bridge care gaps and maintain member communication, health plans need to digitize the member journey. We’re not replacing in-person visits with technology—but we are using technology to inform and support human connections.
Read the Evolution of telehealth
4.
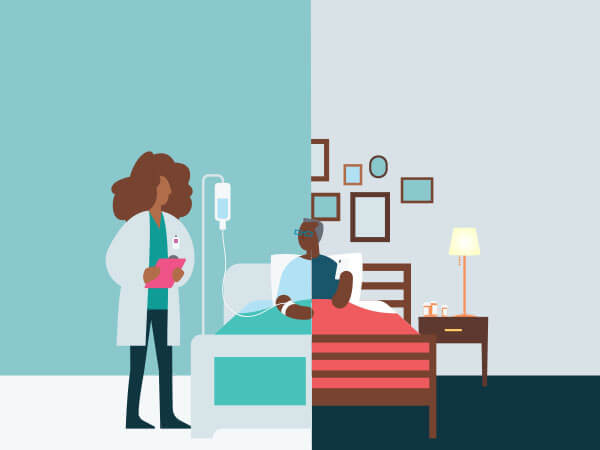
HEALTH PLAN MEMBER IMPACT REPORT:
3 data-backed strategies to improve care transitions
How well is your health plan keeping in touch with members post-discharge? To meaningfully improve care outcomes, health plans need a window into members’ care needs at home. See which member demographics were most engaged with their plans after discharge. Plus, get our 4 key findings on how to reduce readmissions and improve benefits utilization, based on consumer research.
Read the Member impact report

5.
The future of health plan customer experience: 5 critical shifts
What does the health plan landscape look like today? And where should we improve for the future? We explain the 5 most critical shifts we’re seeing in the healthcare industry, from how they look today to where they’re headed tomorrow. Look ahead to prepare for changes in member visibility, digital transformation, and the pivot from volume-based to value-centric member engagement.

6.
Why digital adoption matters to boost technology ROI
Discover what digital adoption truly means for your health plan—and how to implement new technologies in sustainable ways that work for your plan. If you’re unsure where to start, or are having trouble nailing down your goals, this 4-step guide might be just what you need. To get started, all it takes is the right digital health management strategy for the team (and the goals) you have.

7.
Avoid the common pitfalls of remote patient monitoring
Remote patient monitoring is essential to keeping up with member needs after discharge. But it can be difficult for staff and members to keep track of all the tools members use to monitor their health. We highlight 5 of the most common challenges of remote patient monitoring, along with recommendations to help staff stay on top of member communications and data collection.

8.
Does digital health work?
This case study details a new, peer-reviewed method that helps health plans and care managers understand the impact of digital health management on their members. Two similar groups of members living with chronic conditions were monitored over 90 days. Using a digital health management tool led to savings of $641 per member per month, or $1,923 per patient over the three-month study period.
Read Does digital health work?
9.
The reality of seniors and tech adoption
Older Americans are often discounted as being “bad with technology,” or unaccepting of change. But we found that isn’t quite accurate. This fact sheet breaks down common misconceptions about seniors and healthcare technology use. For example, one-third of Americans 64 or older use some kind of wearable device to track their health. Meet your senior members where they are—their phones!
Read The reality of seniors and tech adoption

10.
3 steps to identify and address social determinants of health
Social determinants of health, also referred to as health inequities, are the external factors that impact individual and community health. So how can care managers and health plan staff identify when members are facing health barriers? And what can they do about it once they know? We’ve got you covered in this 3-step guide, complete with a walkthrough of how a digitally enabled workflow can help.