Executive summary
- New, peer-reviewed methodology proved the effectiveness of Wellframe’s Digital Care Management intervention
- Wellframe’s digital health intervention resulted in a 17% reduction in inpatient admissions and a 29% increase in the utilization of preventive medicine services
- Use of digital health management led to savings of $641 per member per month, or $1923 per patient for the 90-day study period
The Challenge
People with chronic conditions face an enormous burden in managing their health on their own between healthcare encounters. Members and their caregivers may have a hard time remembering post-discharge instructions, forget to pick up medications, neglect to schedule follow-up appointments, or otherwise lapse in program adherence. Without visibility into members’ home lives, clinicians and health plans might not know about these difficulties until the member’s health worsens or they are admitted to the hospital. Digital health management seeks to solve these issues.
But the impact of digital health is notoriously difficult to measure, and results may not be attributed to the intervention alone. For example, the group receiving the intervention may be healthier to begin with. Undetermined variables may also affect the outcome, such as social or environmental factors.
For this study, we tested a new methodology using propensity score matching. This allowed us to adjust for known variables and propose a new technique called bootstrapping, or Monte Carlo simulation, to adjust for unknown variables. In other words, we compared two similar chronically ill groups—with one using digital health management and one receiving traditional care.
The Solution
In this study, we compared the impact of digital health management at home on patient care outcomes. Both the control and test groups lived with comparable chronic illnesses—and in most cases, multiple conditions. The difference was that the test group had access to Wellframe’s digital health management mobile app.
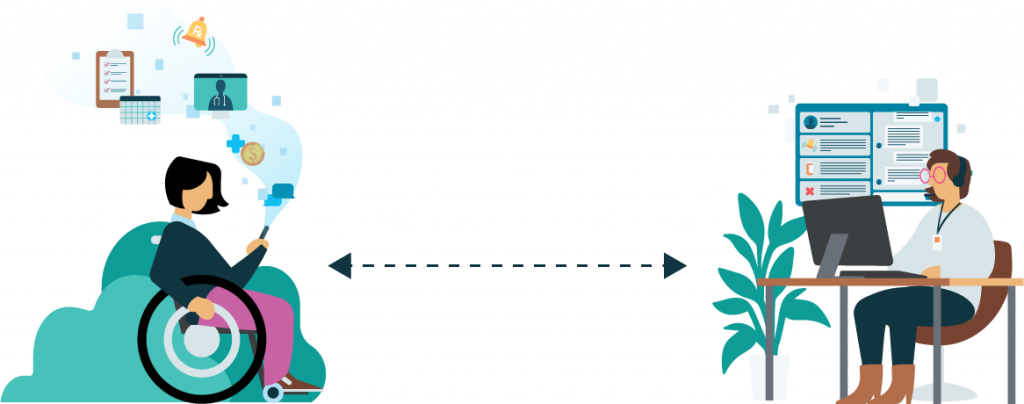
The Wellframe platform includes a mobile application for members and a web-based dashboard for clinical care teams. Use of this secure platform helps health plans reimagine their relationships with members through ongoing engagement.
Members use the Wellframe app to leverage an interactive daily checklist that’s personalized to their needs. Checklists include reminders, surveys, digestible articles, and wellness tips that can help them manage their health at home. As members engage with the app, it shares data in real time with the health plan care team to inform timely support and early interventions. Members can also ask questions on their own time and build relationships with care managers through convenient, HIPAA-compliant messaging.
The Results
The study determined that CR patients who used the Wellframe app showed a significant increase in program adherence and session attendance, across a racially diverse population. Improved cardiac rehabilitation adherence—in combination Participants using the app reported improved care outcomes, which translated to significant cost savings for health plans. App users also reported more frequent communication with care managers and member advocates.
Key stats
- 82-84% of participants had 2+ chronic conditions
- Digital health management translated to cost savings of $641 PMPM, or $1923 per patient over the 3-month study period
- Intervention participants averaged 122 touchpoints throughout the study
In 3 months, members using digital health platform reported:
- 9% reduction in ER utilization
- 17% reduction in inpatient admissions
- 29% increase in preventative services utilization
