The evolution of telehealth: Digitizing the member journey
In the last several months, the U.S. has seen a drastic boom in telehealth usage due to the circumstances created by the COVID-19 pandemic. In fact, the market has seen a 64.3% increase in demand in 2020. Though some speculate that this technology is only a temporary necessity to alleviate the current crises, healthcare consumers say otherwise: 83% of patients expect to use telemedicine after the pandemic ends.
But despite its much-discussed potential, telehealth as we know it is not a digital health panacea: it cannot fill all the gaps in access and support that lead to poor outcomes and low satisfaction. As we look to the continued promise of telemedicine and telehealth, we need to embrace a broader definition of what digital can do to support people during all the moments in between healthcare encounters.

How telehealth is defined today
Often used interchangeably, telehealth and telemedicine allow patients to access primary care and therapy services, as well as to get screened for COVID-19 if they are showing symptoms. Healthcare providers may also monitor biometrics, such as blood pressure and blood glucose, for patients with chronic conditions. Telemedicine can take several forms, according to the CDC:
- Synchronous: Real-time telephonic or audio-visual communication. This is often done by smartphone, computer, or tablet. A nurse or medical assistant may use equipment such as digital stethoscopes or otoscopes with the patient while a consulting healthcare provider conducts a remote evaluation.
- Asynchronous: Patient portals or “store and forward” technology where messages are sent from one device to another, passing through a message center first. The message can be responded to at a later time.
- Remote patient monitoring: The transmission of a patient’s clinical measurements to their healthcare provider.
Where telehealth falls short
Telehealth, as it’s defined today, is subject to many of the same constraints as traditional medicine models — it’s still episodic. We know that 80% of health outcomes are determined by all the factors that happen outside clinical care. But instead of targeting those factors with the contiguous support people need between doctor’s visits, telehealth merely digitizes the visit itself.
Health insurance plans have an important opportunity to extend the reach of virtual health to impact more lives, across more critical touchpoints in the member’s health journey. By embracing a digital health management strategy, organizations can unify resources and education, uncover health insights, and connect members to support on their own time.
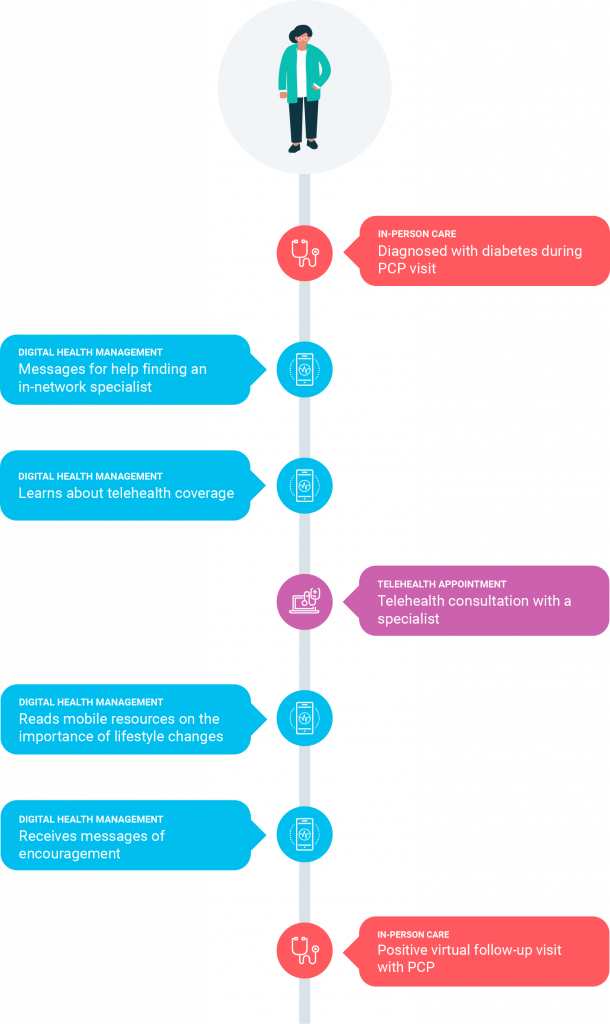
The contiguous digital health journey
Unify resources and education
A 2018 survey revealed that while primary care physicians want to provide high-quality care, 85% admitted they can’t address all of a patient’s clinical concerns and 66% said they can’t address behavioral and social concerns. Leading health plans employ digital health platforms with a wide range of capabilities to address these gaps, whether it’s daily mobile support for lifestyle changes or digestible guidance about healthcare costs and coverage. Among forward-looking plans, these digital platforms may also provide seamless navigation to member resources—including telehealth.
Uncover health insights
Digital health platforms not only supplement virtual visits and provide continuous support, but they can also improve health outcomes by harnessing data from member activity within the platform. For example, mobile surveys can be used to uncover whether a member has recently been diagnosed with a health condition that the plan may not have on record.
To avoid data overload, it’s critical to invest in platforms that can distinguish the signal from the noise to help staff prioritize members based on real-time needs, generate intervention alerts, and recommend next best actions.
Connect members to support on their own time
According to data from Wellframe’s COVID-19 Chronic Condition Patient Population Report, more than half of chronic condition patients have delayed receiving care as a result of the pandemic, either due to their doctor’s recommendations or their own reluctance to go to a medical facility. With the right digital health management platform, health plans can offer their members HIPAA-compliant mobile messaging with health plan staff, ranging from care managers to customer service reps. By meeting members where they are, health plan staff can help members stick with their care plans, monitor symptoms, promote healthful behaviors, or answer questions about healthcare benefits.
Key takeaways
Telehealth should still be viewed as tremendously valuable—it can increase access, alleviate the burden on the healthcare system, and improve member satisfaction with the plan’s offering. Importantly, its accelerated adoption has shifted consumers’ behavior and expectations, opening the door to new possibilities for digital care and support previously not thought possible. We can’t predict how this rapidly changing technology will evolve in the months and years to come. But we do know that health insurance leaders must reimagine how virtual health can serve their members to forge more meaningful connections, across the entire healthcare journey.