How to close the Member Advocacy technology gap to meet member demands
How are health plans using digital health technology to adapt to shifting federal regulations and member expectations? To better understand the motivations and barriers influencing health plan strategy, Wellframe commissioned a survey of health plan decision-makers. We found that most health plan leaders are looking for a comprehensive digital health solution that enables their teams to deliver personalized support. Member Advocacy technology can help.
What is the Member Advocacy technology gap?
There is a rift between the digital experience members expect and what many health plans currently deliver. Health plan members are used to personalized commercial experiences that are powered by technology. The challenge for health plans is providing the customized support members expect without relying on point solutions or overwhelming staff. A Member Advocacy approach can make it easier for health plans to address member needs with technology rather than relying on point solutions
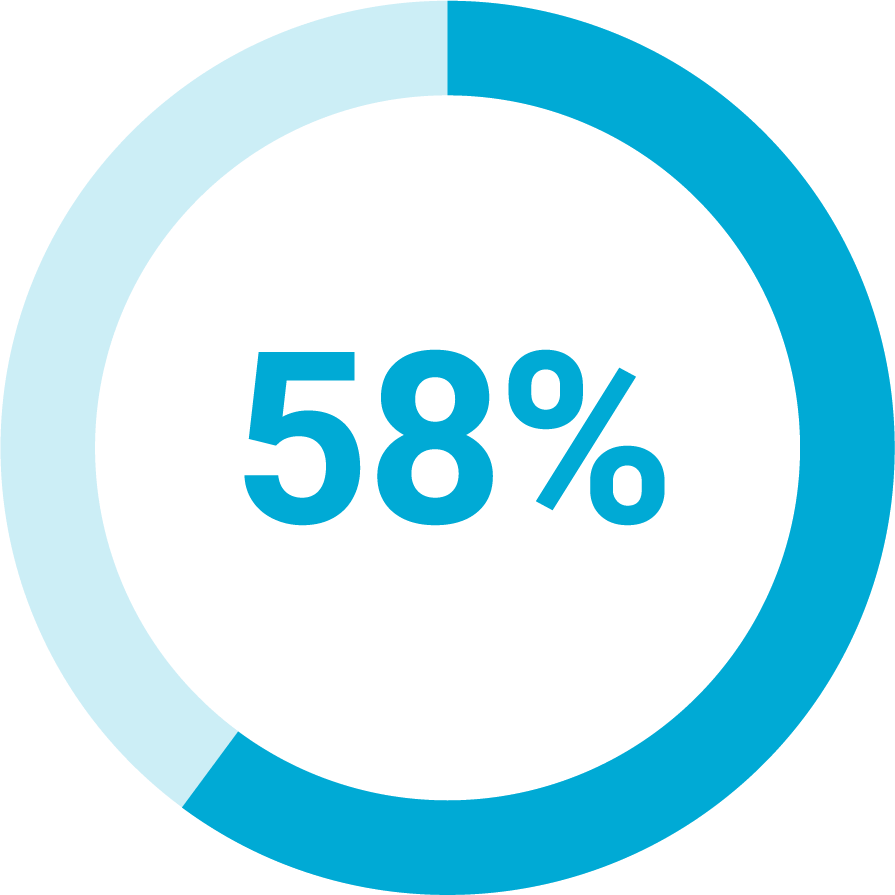
Of health plan decision-makers are dissatisfied with their current member experience technologies.
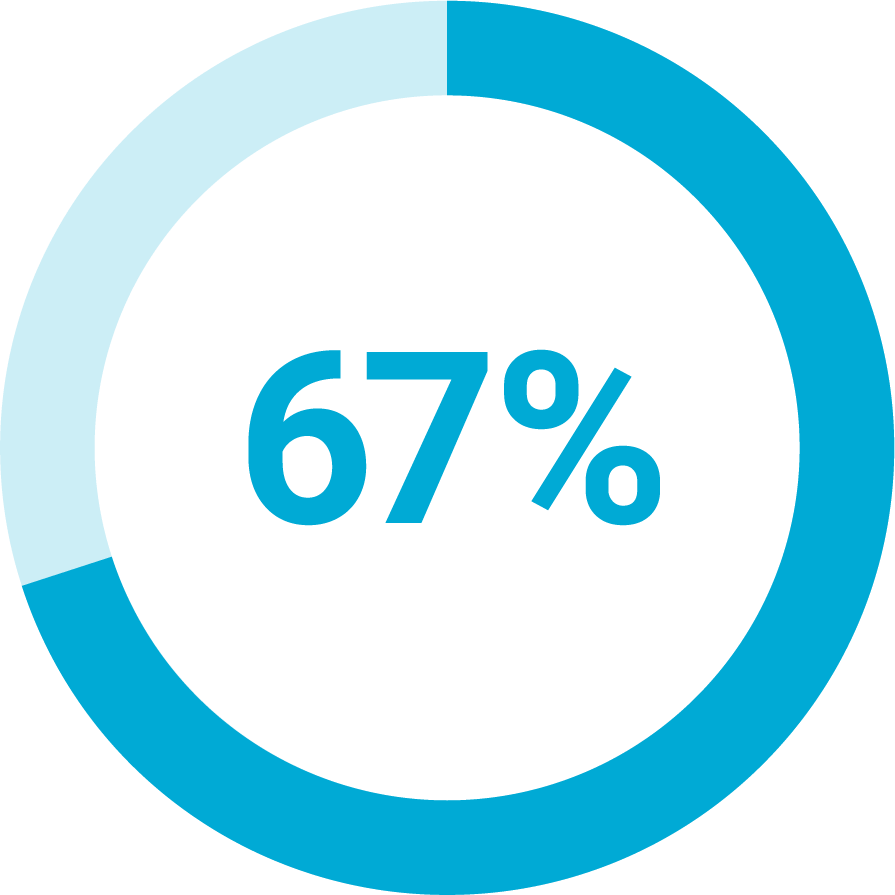
Of payers are working to implement two-way messaging between staff and members.
How can Member Advocacy help your plan deliver personalized support?
More than 80% of health plan decision-makers seek to improve proactive member outreach. But there isn’t a consensus on the best way to understand and get ahead of members’ health needs. Member Advocacy technology supports omni-channel communication, which helps staff and clinicians access near-real-time member information. These insights can make it easier to personalize member support, improving their experience and their outcomes.
According to health plan leaders, there are three primary challenges to closing the Member Advocacy technology gap. Here’s what we learned from asking them about their experiences.

Of health plans support web-based patient portals to address member questions.
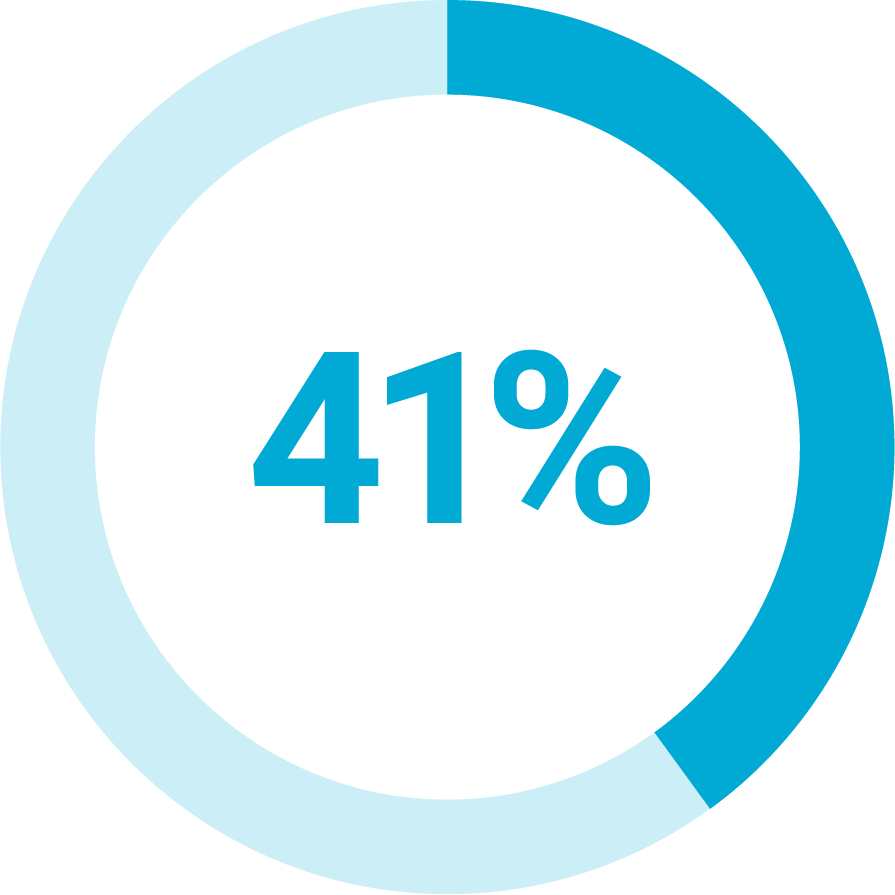
Of health plans attribute slow digital adoption to staff limitations.
Challenge 1: Reduce costs while meeting member demands
Health plans are facing two major shifts in the healthcare industry: price transparency and the transition toward value-based care. To stay compliant with new regulations for member access to health information, health plans must collect new types of data and make it available to members without compromising security.
Currently, payers have the most difficulty collecting care cost and prescription information. For health plans, effectively gathering and disseminating the right information means investing in technology that supports the complex needs of future contracts.
Challenge 2: Align KPIs to provide a better member experience
Two-thirds of health plan leaders are focused on giving members more “one-on-one time” with care managers. Yet more than 55% say their organization lacks a cohesive plan for driving the widespread change needed to achieve this goal. So what is the best way to get your staff on board with Member Advocacy technology and empower them to deliver a better experience? Be up-front about new goals and KPIs from the start.
Our health plan partners recommend tracking and regularly reporting on KPIs such as: weekly onboarded members, number of one-to-one messages sent, and digital touchpoints per managed member.

Challenge 3: Choosing the right digital health technology partner
There is no shortage of digital health technology solutions. But more than 60% of health plan leaders say usability and interoperability are still major concerns. More than half of plan leaders are seeking a single digital technology partner so they can remain in control of their member experience—rather than outsourcing to a third-party vendor.
When looking for a digital partner, payers emphasized the importance of choosing a data-driven platform that can deliver the insights necessary to enable compliance and stay ahead of the shifting healthcare landscape.