As health plans focus on improving the member experience, digital health solutions have emerged as an important budget planning component.
But how should health plan leaders advocate for and prioritize digital care in the context of budget cycles? What are the quantifiable elements of a digital care management solution business case? This guide suggests three fundamental areas:
- Increased staff efficiency
- Reduced medical costs
- Improved quality metrics
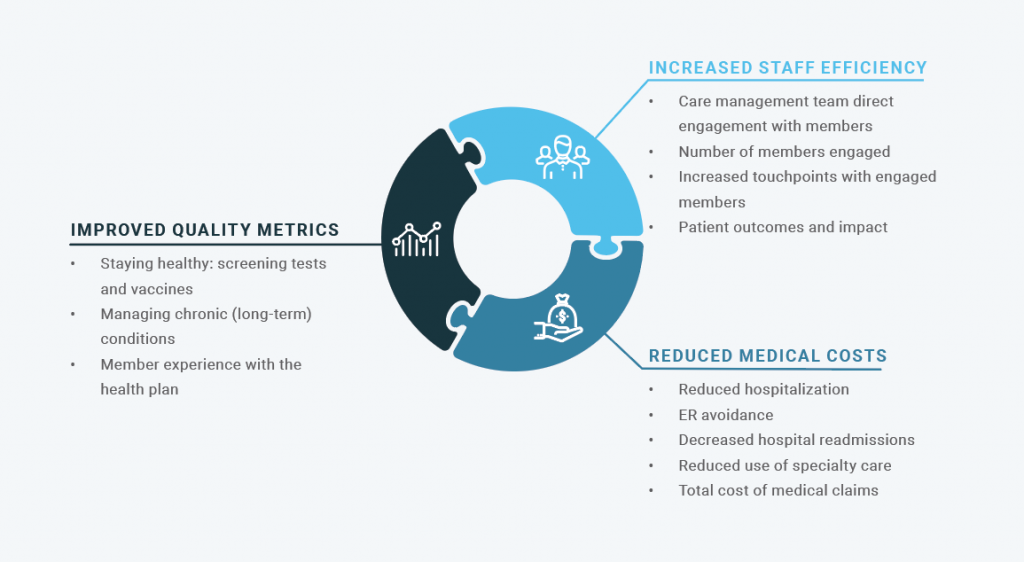
Increased staff efficiency
By incorporating a digital care management solution, health plans can extend the reach of care teams to more efficiently address member needs. Areas of impact that can be incorporated into budget planning include:
- Care management team direct engagement with members — With a digital care solution, care managers spend less time leaving voicemails and playing phone tag and more time directly engaged with members. In-app messaging, for example, offers both a direct engagement channel and an efficient means to schedule and confirm assessment and evaluation calls.
- Number of members engaged — By increasing the efficiency of member engagement, a digital care solution can also enable the same number of staff to handle higher caseloads. Time savings from a digital solution can be applied to engaging additional members.
- Increased touchpoints with engaged members — A digital solution not only allows additional members to be engaged, it encourages increased touchpoints with individual members. Longitudinal support is critical in improving the outcomes of members with clinical conditions. A digital care solution not only enables far more frequent interaction with members, it offers the ability to quantify that interaction.
- Member outcomes and impact — A digital solution incorporating elements such as secure messaging and surveys can provide member-reported outcomes that offer valuable insight into the impact of care management.
Reduced medical costs
Engaged members, supported with longitudinal care — including more frequent touchpoints — and empowered with the ability to manage their health, are more likely to see improved health outcomes and demonstrate more effective utilization. A digital care solution can have an impact on specific member medical costs including:
- Reduced hospitalization
- ER avoidance
- Decreased hospital readmissions
- Reduced use of specialty care
- Total cost of medical claims

Improved quality metrics
There are also specific standard quality metrics which health plans are already measuring that a digital care solution can impact. A digital care solution can help health plans capture valuable enrollment revenue and additional bonus payments by:
- Delivering omnichannel support to help members stay healthy
- Supporting the whole person to help members manage chronic conditions
- Making the health plan member experience easier to navigate
These elements of a digital care solution can impact numerous quality metrics including:
- Staying healthy: screening tests and vaccines — By meeting members on their terms, providing education and identifying potential barriers to care, care managers can help members ensure they’re scheduling follow-up appointments, and taking actions that help meet star measures for screenings, vaccines, and other check-ups.
- Managing chronic (long-term) conditions — When health plans deliver holistic, comprehensive support that is personalized to members’ needs, members will feel more engaged in their care plan and have a better understanding of why and how to adhere to their treatment protocol and prescribed medications. This makes health plans better positioned to meet measures for chronic disease management.
- Member experience with the health plan — By giving members a clear point of contact for the plan and addressing and prioritizing their needs, members will feel better supported and be more likely to respond positively on the overall rating of their health plan.
Click here to download the full Wellframe Star Ratings guide.