
In 2023, more than 70% of Medicare Advantage members are enrolled in plans with a rating of 4 or more stars. Though this is a decrease from 2022 (86%), it’s consistent with enrollment in 2019 (72%), before emergency insurance coverage measures were put in place during the COVID-19 pandemic. With coverage rates falling to pre-pandemic levels, your health plan must be more focused than ever on improving quality and member experience.
Health plans with ratings that slip below 4 stars are at risk of financial losses from decreased enrollment rates. Lower ratings also lead to reduced ACA rebates, and lost ACA bonus payments. Digital Care Management and Clinical Advocacy solutions can help your health plan improve quality measures, recapture enrollment revenue, and secure bonus payments.
In this guide, we outline the steps your organization can take to improve your Medicare Star Ratings success:
- Step 1: Deliver omnichannel support to help members stay up to date with their care
- Step 2: Support the whole person to help members manage chronic conditions
- Step 3: Improve healthcare navigation and the member experience
Raising Star Ratings from 3.5 to 4.5 stars could increase CMS rebates by 45%*
Step 1: Deliver omnichannel support to help members stay up to date with their care
Star Ratings category: Timely & effective care
Your members want options for convenient, omnichannel support when it comes to managing their health. More often, we’ve heard members talk about their preferences for self-service and asynchronous communication. Offering a variety of health education and outreach tools allows members to get in touch when it’s convenient, instead of playing phone tag. They can also access more frequent support and guidance using a digital tool compared to intermittent phone calls.
This shift to omnichannel health management also helps support care managers. With digital health management tools like care programs, surveys, and 1:1 messaging, care teams have the tools they need to develop long-term relationships with their members. Earning members’ trust can improve member experiences and retention—leading to higher Star Ratings.
Here are examples of two member journeys:
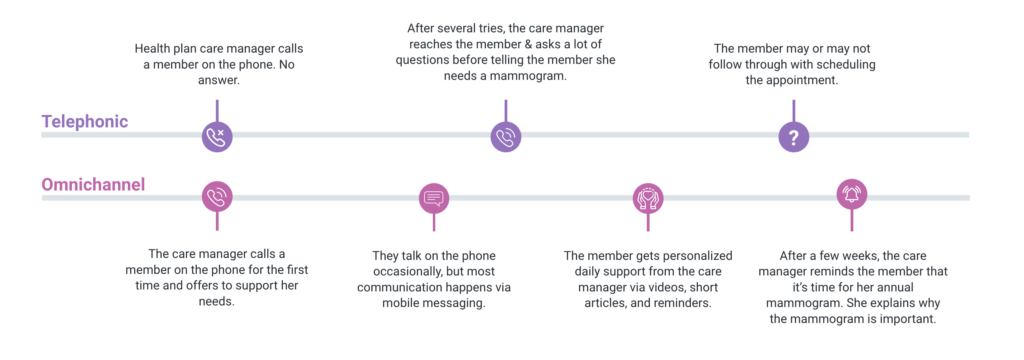
Telephonic
- Health plan care manager calls a member on the phone. No answer.
- After several tries, the care manager reaches the member & asks a lot of questions before telling the member she needs a mammogram.
- The member may or may not follow through with scheduling the appointment.
Omnichannel
- The care manager calls a member on the phone for the first time and offers to support her needs.
- They talk on the phone occasionally, but most communication happens via mobile messaging.
- The member gets personalized daily support from the care manager via videos, short articles, and reminders.
- After a few weeks, the care manager reminds the member that it’s time for her annual mammogram. She explains why the mammogram is important and helps her schedule an appointment.

Insider tip:
It’s easier to engage members in their health by providing value up front with easy-to-access resources and communication tools. Once care managers can engage with members, they can hold members accountable for achieving their health goals.
Step 2: Support the whole person to help members manage chronic and comorbid conditions
Star Ratings category: Readmission
To help reduce readmission rates, health plans must think beyond the episode-driven approach to condition management. What does it mean for health plans to support the whole person? Give members access to their full care teams and resources that empower them to address the clinical and social factors that impact their health.
How do digital health tools help reduce preventable admissions and provide whole-person support? By delivering personalized health management education and care programs that address social determinants of health along with clinical needs.
Meet clinical needs and social determinants of health
Reducing readmissions starts with proactive intervention. Instead of waiting for claims data to come in and following up with members after a clinical episode, many health plans are leveraging digital health management tools to uncover gaps in care—before they lead to complications.
Digital health solutions like Wellframe offer digital surveys and assessments that screen for intervention points and unmet health needs. Care teams can use information from these surveys to prioritize outreach to their highest-risk members. Clinicians can also combine answers from digital surveys with information from 1:1 messages and previous member conversations to deliver more personalized support.
Address comorbidity with comprehensive clinical programs
About 3 in 5 Americans live with multiple chronic conditions. And, according to a Wellframe survey, 1 in 3 members with a chronic condition are overwhelmed by managing their health. Make it easier for members to take control of their health now and prevent complications (and readmissions) later.
Making digital care management programs available to high-risk members can extend the reach of care teams while delivering relevant and timely interventions. Some of the care programs Wellframe customers leverage most often include diabetes, maternal health, transitional care, and behavioral health.
Insider tip:
Members feel more engaged when health plans offer comprehensive support, and have a better understanding of why tests and treatments are necessary. This puts health plans in a better position to improve Star Ratings.
Step 3: Improve healthcare navigation and the member experience
Star Ratings category: Patient experience
Members’ experience with your health plan is another critical component of your Star Rating. Many members have a confusing and overwhelming experience with a health plan. This makes it more difficult for members to ask questions and have their needs met.
Consider implementing a coordinated, one-stop experience for members. This can reduce frustration and better meet the member’s needs. This can also improve your ratings on Medicare’s member experience survey.
A centralized member experience
As part of a larger digital health strategy, a Clinical Advocacy solution can ease or eliminate major healthcare obstacles for members. Obstacles include appointment booking, finding a provider, and verifying benefits coverage. As a result, members may postpone care or make choices that are not cost or quality effective.
Clinical Advocacy can organize and unify information in a way that is engaging, relevant, and accessible to members. This type of offering also provides members with a single access point that makes it easier for them to address diverse needs. Plus, it can help break down internal communication silos between care teams and administrators, facilitating communication to better address member needs.
Insider tip:
Members will feel better supported once they have a clear point of contact. They’re also more likely to respond positively when asked to rate their health plan.
Key takeaways
Without digital engagement, it can be nearly impossible for health plans to access the near-real-time member information they need to deliver the personalized, proactive support that improves clinical outcomes and the member experience.
Even gradual improvements to Star Ratings can help health plans attract new enrollees and expand market share. That can translate into additional bonus payments.
Position your organization for success this reporting year by taking the following steps:
- Deliver omnichannel support instead of telephonic-only outreach. This encourages members to get screening tests and vaccines.
- Address the needs of the whole person, rather than single episodes of care, to help members better manage conditions and reduce readmission.
- Make it easier for members to navigate the healthcare system and improve the member experience.

Would you like to hear how other health plan leaders have been able to improve care outcomes, lower costs, and improve member relationships for Medicare members?
Watch our on-demand webinar, “Support Medicare Members with a Digital Ecosystem”