Should you build, buy, or partner for a Member Advocacy solution?
More than 50% of consumers would rather wait at the DMV than deal with a health insurance issue. So it’s no surprise that digital-first organizations are gaining popularity. Your health plan could use that to your advantage and outsource to these competitors. Or you can improve member experience without relying on third parties. What’s best for your health plan—to build, buy, or partner for Member Advocacy?
Jacob Sattelmair, DSc, MScWhen it comes to Member Advocacy, many plans see two bad options. Partner with a disruptor and hollow out the competency, or retain ownership but struggle to modernize quickly enough to compete.
Wellframe Co-founder, Executive Vice President and General Manager
What to look for in a Member Advocacy solution
Choosing the path that’s right for your health plan starts with understanding your goals. Gather your key stakeholders and ask questions like:
- Is your focus on administration, member experience, or something else?
- Are there aspects of the member experience you want to outsource?
- Does your current solution have the appropriate infrastructure to scale?
- What is your organization’s roadmap for the next 5 years?
- Which resources does your health plan have to build and develop new technologies?
Answering these questions early will help you pick the vendor that best fits your needs—and your budget. They will also help you set implementation milestones so your team stays on track.
So what are your options?
Jacob Sattelmair, DSc, MScPlans enjoy many structural advantages relative to their ability to deliver a high value advocacy service. They have access to lots of data, provider relationships, employer relationships, they have scale, can be creative in pricing, etc. But plans’ slowness to improve has left a void that is quickly being filled by new entrants.
Wellframe Co-founder, Executive Vice President and General Manager
Options for implementing Member Advocacy
1. Outsource to competitors
One option is to outsource your technology ownership to a third party vendor. The vendor takes responsibility for implementation and rollout to members. That gives your health plan more time to focus on other initiatives. This option may feel the most like a “plug-and-play” solution.
The downsides to outsourcing is that it may erode brand loyalty over time. It could also diminish members’ perception of your value. Your vendor controls member-facing technology and member experience. This means the technology your members use would feature their branding, and members would be talking to the vendor’s support team. Plus, once you choose a vendor, it’s harder for your organization to shift course without starting from scratch.
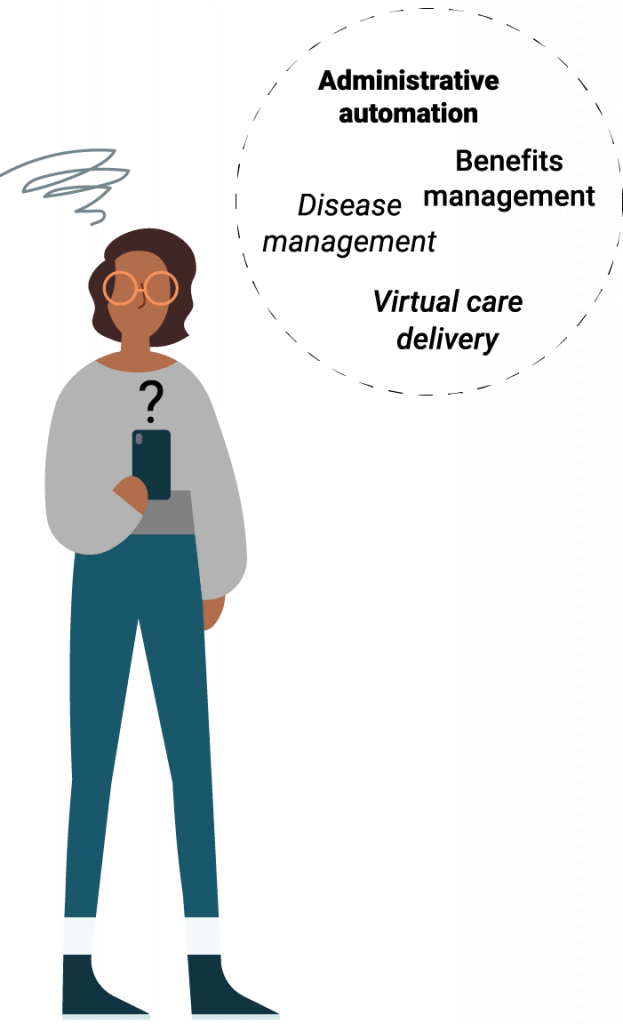
2. Rely on point solutions
Another option your plan has is to create a custom suite of point solutions. This allows you to pick the individual vendors and technologies that serve your needs. You could choose one vendor for secure video calls, one for patient portals, one for staff efficiency, several to address specific chronic conditions, etc.
However, this creates a few separate issues. The primary concern is interoperability. Your team would have to ensure the technologies work together without costing extra time or money. Using point solutions may also overwhelm members and customers. Multiple solutions means keeping track of multiple apps and login credentials. Offering a fragmented experience like this could negatively impact user experience.
3. Build your own platform
Building your own platform would let you create the most customized technology based on your needs. All customer- and member-facing experiences would center your brand. And all member and staff experiences would be with your staff.
But there are reasons more health plans don’t try this approach. Because you’re building a technology solution from scratch, it will take longer to bring it to market. Custom solutions are also resource-heavy, and can be expensive. Building new technology requires input from developers, designers, data scientists, and other experts.
4. Choose a proven partner
Finally, your health plan has the option of choosing an established technology partner. A true partner can offer a proven platform that you can customize based on your needs. This could include co-branding, which can improve member loyalty and build trust.
A partner may also offer content libraries and a member benefits hub. Some partners also help you with member marketing, which can help increase awareness, adoption, and engagement. Partnering can help scale your vision while ensuring you still own member relationships.
Anonymous Wellframe userThe Healthcare Nurse assigned is always helpful. The checking off of doing my tasks makes me feel accomplished. The articles can be super helpful, and the exercise tracker makes me feel so happy when I accomplish the goal.
Why should you partner to implement a Member Advocacy model?
Navigating the healthcare system can be overwhelming for members. And understanding what members need can be overwhelming for health plans. Partnering with a proven vendor can help your plan deliver a modern member experience and improve outcomes. By working with a customizable platform, you can help staff extend their reach and uncover valuable member insights.
Member Advocacy encompasses a wide range of technology and workflows. And your plan doesn’t have to build a solution from scratch to find the perfect fit. Partnering allows you to combine technology, content, device integrations, and data science. Give members the personalized care they deserve.