What is FHIR?
The Fast Healthcare Interoperability Resource (FHIR) is a standard and set of guidelines that dictate how information is presented and transmitted. In simplified terms, FHIR (pronounced “fire”) is an agreed-upon language into which information is translated so it can be easily shared across disparate platforms and systems. This system allows for the secure exchange of clinical, administrative, and other healthcare information.
FHIR determines three key guidelines: what format data is in, specific phrasing and definitions for terms, and the technologies supported in data transmission. The common language makes it easy to access the data and submit queries. Streamlining the format in this way maximizes the value of shared data.
For example, FHIR dictates that all patients be referred to as “patients,” though other organizations might call them “members” or “program users.” Similarly, what FHIR calls “practitioners” may elsewhere be referred to as “doctors,” clinicians,” or “care managers.”
“The challenge with healthcare is that data has always been locked behind silos with two strong limitations,” says Mohammad Jouni, Chief Technology Officer at Wellframe, “1) No incentives for the data owners to share the data externally and 2) no common technology and services that make it easy to store and move the data around.”
Data storage is moving from static servers and physical drives to cloud- or web-based storage. FHIR enables this shift in information storage and exchange.
Why is FHIR the new interoperability standard?
“One of the key ways to enable innovation in an industry is to make sure that data – with the proper authorizations and privacy protections in place to protect the end user – is easily accessible to entities who can think of new ways to add value using that data,” says Mohammad Jouni, Chief Technology Officer at Wellframe.
Because FHIR is based on pre-existing standards used to transmit data, the barrier of entry for new software is lower. In other words, developers have experience in how data is securely transferred, so it’s easier to adapt those transfer methods to the healthcare industry than to start from scratch.
Another way exchanging information is made easier is that FHIR removes all metadata. Doing so separates a person’s understanding of the data from the data itself, and enables the cleaning, sending, and interpreting of information across systems—and eliminates costs associated with this process.
While metadata can be useful for giving context to your data, it also creates bulk when storing and transmitting information. Excluding metadata in this context allows for unclouded analysis of raw data. Analysts can still reference the metadata without the added work of separating it from the original data.
FHIR also solves some deeper problems. Only non-proprietary data formats are supported, which makes the shared information accessible to a wider audience. Users don’t have to worry whether a recipient has the proper application to open and read a report sent using FHIR. The system is also endorsed by the U.S. government, specifically the department of Health and Human Services (HHS), simplifying the integration approval process when sharing data.
Organizations outside of healthcare are adopting FHIR based on government endorsement and the knowledge that using a common language saves money. Some of these companies include Apple, Amazon, and Google.
How does FHIR impact quality reporting?
HEDIS performance measures are designed to track improvement in care outcomes and delivery. This includes preventive care, long-term care management, care access, member experience, healthcare utilization, and other areas.
The National Committee for Quality Assurance (NCQA) tracks digital HEDIS measures. Digital quality measures leave less room for human error due to interpretation and retyping. In addition, digital measures make data transfer faster and easier. FHIR enables this kind of digital data transfer by streamlining the information and making queries simple.
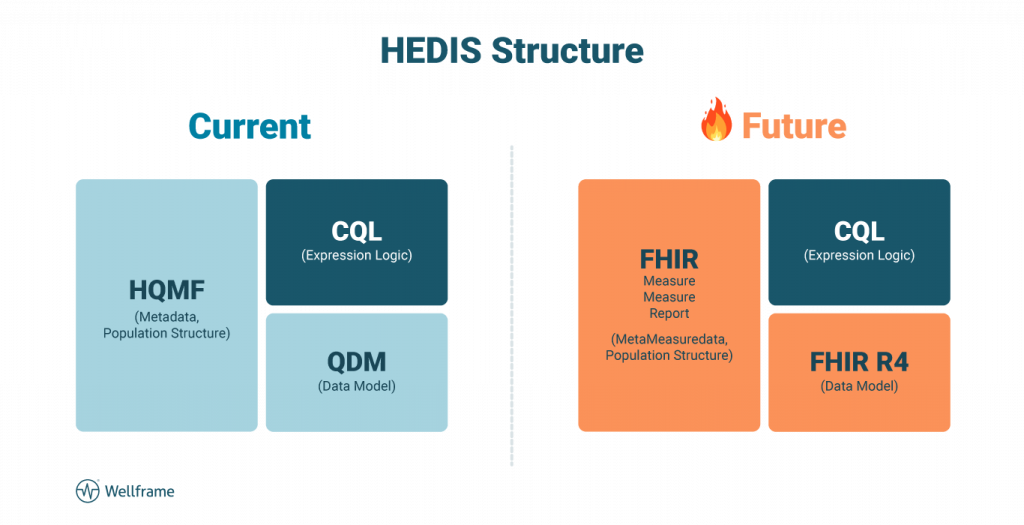
For these reasons, the NCQA HEDIS structure is shifting. The current structure includes Health Quality Measure Format (HQMF), Quality Data (QDM), and Clinical Quality Language (CQL). The future HEDIS structure aims to replace HQMF and QDM with FHIR modules. Instead of using HQMF for metadata and population structure, NCQA will use FHIR MetaMeasureData and population structure. Similarly, the QDM will be replaced with the FHIR R4 data model.
There are five levels to the FHIR framework. Levels 3 and 4 are most relevant to quality reporting, as they encompass administrative, clinical, diagnostic, medication, workflow, and financial data. Because this information is all in the same FHIR “language” with no metadata, the information can be queried easily.
As an example, data analysts can run a report to find the age of every patient diagnosed with diabetes. This search could be limited to a certain location, or be broadened to include the entire U.S. While much of this shared information may appear to be digital exhaust, it can be incredibly useful under the right lens.
When patient, hospital, and practitioner information is all in one place—and is reported using the same vocabulary—it’s easier to access data from various hospitals, health systems, and patient populations. Even outside of traditional reporting, data analysts can pull key insights about diagnoses and demographics about other populations for comparison.
What else can FHIR do?
Primarily, FHIR is intended for use as a base platform, to be customized and built off of. It allows for a base understanding across all users, ideally leading to true interoperability across the healthcare industry. Rather than having one app that does everything, FHIR offers a basic starting point for developers to create unique apps and services for.
This feature also makes FHIR a good starting point for artificial intelligence (AI) development. All the data that can be used for training a machine learning solution is already in one format. Developers don’t have to spend extra time cleaning data to feed the AI—they can jump right in with the information that matters most.
As you’re planning your digital roadmap, make sure you’re building around member experience to truly future-proof your health plan. Offer members an integrated experience, whether they’re meeting with clinicians via telehealth or managing multiple conditions at home. Building on a platform that leverages FHIR-based APIs means you can be confident knowing you can adapt to a changing landscape with new tools and services that meet shifting member demands.